cw: birth/medical trauma, body function realness, and some well-placed profanity. there’s a tl/dr at the end if you don’t have the time, interest, or attention span for a long one…
***
this story, like most other birth stories in my experience, is equal parts magic, terror, transformation, strength, grief, and joy, and most like most other birth stories, it reflects an experience that i never could fully have imagined until living it. as a midwife, i always tell clients, “yes please, make a birth plan, and yes please, vision your ideal birth, but then and perhaps most importantly imagine that plan as the absolute roughest of guidelines, a loose and curious request of sorts to the universe, knowing that babies have their own plans and that so much about birth is about letting go of expectations and (most especially?) of the illusion of narrative control.”
this reminder, like so many other pieces of midwifery advice i’ve given others a million times, i tried to give myself and to truly take to heart. i’ve always known intellectually how difficult the “expectation versus reality” balance is in birth—i’d walked strange and powerful walks through the unknown with so many others before—but my own birth invited me to feel it more deeply on a spiritual and emotional level and, you know, actually do it.
i’m beginning to write this story almost six weeks to the day after giving birth. i got a basic story skeleton down in my hazy first week so that I wouldn’t forget anything, but if you’ve shared space with a newborn of your own, you know that accomplishing anything besides roughly a quarter of the basic tasks of daily living in those early weeks is a great big NAH. i haven’t showered in three days, i’m wearing a nursing shirt covered in milk (new and used) and a pair of my husband’s old thermal underwear pants (freak june cold snap), and my glasses feel alien on my face after so long not needing them. i’m sitting at the kitchen table eating the last of the meal train spoils, and my daughter ruby, my birth story muse, is sitting in a baby seat beside me. she’s mowing down on a binkie after a milk snack, and we’re listening to “womb sounds” over the big speaker. the heartbeat and rushing water sounds calm her down, and i must admit they’re pretty hypnotic for writing as well. (as a side note, stephen and i get a kick out of how borked our spotify mixes are now that night times require endless queues of womb sounds and white noise.)
emotionally, i’m both completely in love, deeper than I ever knew possible, and working hard to be gentle with myself as i, an independent and spontaneous wanderer for 41 years, navigate the intense (and temporary) new limitations of life with a newborn. mentally, I’m starting to come out of the fog and am beginning to bring (a little) more executive functioning back online. the story that I’m about to share with you i share through the lenses of a six week remove, a beautifully humbling case of “milk brain”, and a reckoning of events that took place in an intensely sacred and wildly outside-of-time liminal space. i promise to do the story my best justice, and please forgive any lack of clarity or of elegance in my writing—i plead insanity by reason of unslept new motherhood, and i will be pausing every other sentence to give a wayward binkie a poke back in the right direction.
april 28, 2023, a friday
on the friday before my birth, i visited one of my very favorite places in the world: diana’s baths. despite being floored for the first trimester (plus) by nausea and migraines, i’d managed to stay active in my third trimester with flattish hikes and woods wanders, and the baths was a place that i’d wandered often. there’s a bathroom (YUGE pregnancy plus), the trail is uncommonly easy and spacious, and the payoff at the end of the short hike is a stunning cascading falls accessible via a rooty and perpetually wet terraced trail that seems to climb upwards forever. there are always loads of people there, and while that’s typically an annoying feature, this time it felt like a comforting add-on to a hike at 41 weeks and 2 days pregnant.
as i waddled out and back twice, i took time to appreciate the smiles and occasional comments of passersby. even though it’s always good advice never to comment on someone’s body, especially a stranger’s, i found myself soaking up public recognition and commentary at the end of pregnancy. i think that working so incredibly hard to get where i’d gotten meant that i wanted to be seen as having done it. the fact that i absolutely loved my pregnant body also helped. i loved the shape, the feel, the permission to take up space. so good! am i pregnant? fuck yes i am, and it was a lot of work—thank you for seeing me!!
a recent history of intense hiking and run-training meant that my body hugged my baby close, never quite giving away how far along i was. (great for postpartum bounce-back—not so great for breathing in general or for avoiding heartburn). one lady i passed (i guessed her to be in her eighties) said, “oh, bless you out here hiking like that. when are you due?” when I said “nine days ago” with a smile, she expressed exaggerated but lighthearted mother-hen concern for me being out “in my condition”. (my “condition”, i thought, was very pregnant and very bored and very interested in continuing to keep a mild and incredibly recent case of gestational hypertension at bay).
the falls at the end of the shady, pine-wooded path were as beautiful as ever, raging and high with the april rainfall, and as i wandered around, up the root steps and between boulders, i remembered dipping my toes in the baths the day after my positive pregnancy test back in august. “getting ready for the first of ten pregnancy full moons with a dip in the baths” the photo caption of my sandaled feet in the water had read. how fast those ten moons flew by.
towards the upper reaches of the falls, where the trail crowd transitions from day-tripping, sunburned flatlanders to longer haul hikers and curious explorers, i passed a sporty-hippie vibe kind of man with a new baby of his own strapped to his chest. “hey, good luck!” he said as we met eyes. “you’re gonna do great!”
for the whole return waddle, i beamed.
***
throughout the latter half part of my pregnancy, friday night was date night, a tradition that stephen and i started both to spend time with one another and to get the most out of our soon-to-vanish ability to go out to eat anywhere on a whim, so after my walk to the falls, he and i met up with three friends at a local restaurant and pub. dinner was delicious and company was superb, but the thing that i remember most was what it felt like that night to sit on a hard chair. bean had been riding pretty high in my belly all throughout the end of my pregnancy, but that night, i felt her drop down low in my pelvis. it was such an odd sensation, and the achey/burny pressure down from her head plus the unyielding metal hardness up from the chair put my entire undercarriage to sleep.
finally standing up after a long dinner on a hard chair was a festival of zings, and the increase in pressure i experienced walking back to the car was uncomfortable but productively so, kind of like like a hard massage on a sore, overused muscle after exercise. i can’t think of a better way to describe it. shortly after we got home, i started to feel crampy. i had the feeling that labor would start soonish, and i was thankful to have a beautiful walk and a big dinner on board. to bed we went.
april 29th, a saturday
(real-time author note: second day of writing, frequently one-handed typing because bean needs rocking to be soothed. once again at the kitchen table, same outfit as yesterday but with brushed hair and teeth (winning!), pumping after a feed with a medela pump-in-style that I have just noticed, hilariously, is covered in coffee. i call this tableau “still life with newborn.”)
my alarm clock of sorts saturday morning was the sensation of an actual labor contraction that broke through the haze of sleep—they continued incredibly mild, irregular, and infrequent, but unmistakable in their start-build-peak rhythm. there was also a hint of low back ache, which can be very normal. i was surprised to have gotten a full night of sleep after the crampy post-dinner prelude. that surprise is a feeling familiar to midwives who go to sleep waiting on putzy labors to kick in and then wake up the next morning frantically checking to see if they missed a call. bodies love to start things at night and then fizzle out once sleep takes hold.
with the potential for actual labor looming, i cancelled plans for the day, sent stephen to work (first labors generally have a notoriously long build-up), and got to the business of last-minute pre-birth prep. readying a space for a birth, especially a water birth, can be a challenging balance of prognosticated preparation—set up a birth tub too soon and the cat will terrorize it to dramatic effect; set it up too late and you have a stressed partner and/or a baby being born into six inches of water because “i want my waterbirth, damnit!” (true story). since things weren’t going guns blazing, i saved the tub and the toilet bleaching for stephen (lucky him!).
daylight, as it frequently does, dispelled the labory sensations by about noon. There was a quiet rest of the afternoon and evening while i puttered around the house.
***
contractions started back up just after 8:30 that evening, still irregular and mild but now a bit closer together. my contraction timer, which i began using just before 9, clocked them at varying frequencies between 7 and 17 minutes apart, and interestingly, they were 1.5-2.5 minutes in duration right from the start. no sweet little 15-30 second warmups for me. the discomfort in my back returned, this time just a tad more intense than before, and when i palpated my belly, i felt all arms and legs, meaning that bean had settled into what’s called an “occiput posterior” or “op” position. she was head down (yay!) but her back was to my back with limbs and face forward-facing (boo!). for an easier and more comfortable labor, we want backs out front and babies facing parent’s spine. bean had been super mobile throughout the end of pregnancy, so i didn’t sweat it too much and started moving through some positions intended to encourage a better anterior position—”miles circuit” to birth nerd readers.
by 10pm it was clear that early labor was likely here to stay, so i told stephen he should probably head to bed with me. by 11 contractions had started coming more regularly about every 15 minutes and were lasting around 90 seconds. during a trip to the bathroom i noticed lots of bloody show, which is normal, healthy bleeding from burst capillaries on the cervix as labor contractions cause it to thin and dilate (picture the top of the uterus bunching and pulling up on the bottom segment, pulling the cervix to and eventually over the top of baby’s head like a too-tight turtleneck). most importantly, bloody show is an external sign that internal change is happening. wheeeee!
i reached out to my midwives via messenger to share the info and then continued dozing in bed between contractions, moving my body from deep knee-chest to extended side-lying and back again to encourage a change of position from bean. this was another “practice what i preach” midwifery moment for me, as began to think “yes, please, more of that!” with the start of every contraction. inviting softening, inviting opening, inviting sensation.
april 31st, , a sunday
the slow and sleepy hormonal soup of nighttime kicked things right along. just before 2:30am i messaged acadia, one of my midwives, to say that contractions were now every 8 minutes, lasting 120 seconds, rated mild to moderate, and had loads of mildly uncomfortable low back sensation. i was still dozing and coping super well. stephen and i carried on getting rest.
just before 5am, things really ramped up, and it was clear that the additional sensation i was experiencing was likely “back labor”, a phenomenon that we don’t understand very well where contractions are experienced partially or primarily as mild to extremely intense low back pain. it’s more common with op babies (baby’s back to parent’s back), and the thought is that the pain originates from the pressure of the back of baby’s head against the inside of the parent’s sacrum. normally, an anterior baby (baby’s back to parent’s front) has the soft parts of their face tucked into the cupped curve of the sacrum and coccyx, with the hard back of the head pointed at the soft and pliable tissues of the pelvic floor. when baby is posterior, it’s bone on bone, and each contraction presses hard tissues together, which can be horrendous for the parent—i can’t imagine it’s much fun for the baby either.
my update message to acadia read “back labor blows”. i had some relief options on deck but decided to hold out on the tens unit and the tub until good strong active labor, because relief is never as, well, relieving as it is the first time you use it, and i didn’t want to blow that resource by employing it too soon.
sensation continued to increase towards more of an active labor pattern, with waves of intensity coming every 4-5 minutes and lasting a full 2 complete with increasingly intense back pain. i messaged acadia that “i could use a person”, and i asked her to bring supplies for sterile water papules, little intradermal blister-like injections of sterile water (think old-school tb test) in the skin over the low back that burn like bee stings but are meant to distract the brain from deeper pain. (this mechanism is called “gate control theory”, and you use it every time you rub your shin after running it into a coffee table or when you kiss a child’s booboo after they fall).
acadia arrived just before 7, life-giving coffee in hand, and while the whole team of midwives had been planning to attend, brenda and grace were called to another birth that same morning. another local midwife was on deck to assist, but for a first baby, there’s no point in calling an assist too early lest you all find yourselves in a multi-day campout and exhausted once it’s go-time, so stephen, acadia, and I carried on just fine as a team of three.
the next couple of hours were a heroic effort on the part of the birth team, going through all of the pain relief measures we could think of for a back labor that was becoming more and more intense. with each contraction, in addition to the manageable and expected intensity of uterine contractions, there was a stabbing pain in my sacrum, and as contractions carried on, it stopped being a start-build-peak-release pattern with the back pain and just came full-on instantly intense with the start of each contraction. off then on, like a light switch of doom.
we tried sterile water papules—they didn’t work (they don’t more than half the time in my experience). the initial intensity of the sting did overwhelm the back pain at first, but once my body acclimated to it, the effect vanished completely. It was an interesting academic experiment though, so I was glad to have tried.
then we tried counter pressure (pushing back with a flat hand on the sacrum to counter the push from inside)—it didn’t work and actually made it worse, which was very surprising to me given how many people I’ve seen love (and even frantically demand) counter pressure to relieve back pain in labor.
then we tried the tens—it didn’t work either. i’d had such high hopes for this one, but the buzz-buzz-BUZZ of the electrodes on my low back pushed the overstimulation button in my brain big time, and I was pretty frantic about wanting them OFFFFF NOWWW. (fun story: this one had been a bit of a comedy of errors anyway since we didn’t realize it required 10 hours of charging out of the box rather than taking batteries or plugging in. i was worried that i wouldn’t have access to one of just a few non-pharm methods of pain relief because of the charge time, but it turned out that a) 2 hours of charging was enough for some basic use, and b) it, sadly, felt horrible anyway).
with contractions coming every 4 minutes and lasting 2, i moved around the house looking for a place or a position to maximize what little reprieve i had from the slowly increasing sacral stab. all my moving and shifting didn’t seem to want to budge bean from a posterior position, so labor became more about just managing that sensation. as a midwife, i’m always fascinated to see what positions and places people settle into, what they fixate on, and what rhythmic rituals they employ for the purpose of coping. it’s rarely what you’d think, and when someone finds it, you just have to go with it. my place was our living room (we call it the “great hall”) kneeling in and leaning over the back of a stuffed chair. i gripped the patterned cloth of the chair back, my cheek and chin resting on the chair between my hands. when the pain became too intense, I would stretch my right leg back behind me to touch my bare big toe to the floor, positioning my hips in an asymmetrical stance, begging bean to take the hint and make the turn to anterior. rinse repeat. rinse repeat.
my visual fixation was the pattern of the upholstery, and with each back labor contraction, i deepened my forward-lean and whisper-breathed the word “relaaaaaaaax” to myself as i tried to cope. one time in this position (and two or three other times during my labor), i felt bean shift a bit and i got to experience “just a normal” labor contraction—it felt so good, strong, productive, and intense but manageable—a relief in comparison to back labor. such a shame that the shift vanished just as soon as it came on.
as i labored there, i received perfect, simple, quiet encouragement from stephen—a balm compared to the overstimulation of the physical comfort efforts i’d been so sure would work. he popped in and out of the great hall to check on me as he and acadia undertook the task of filling the birth tub—a project that takes more time than you’d imagine and pushes poor hot water heaters to their absolute limit. i’d thought about trying the shower, but acadia suggested that starting the tub project might be a better use of the hot water. i stayed in my coping spot on the chair while they prepped the tub.
the other love-it-or-hate-it labor location is the toilet. i, like most, veered more towards the “hate it” camp because while it brought on stronger and more frequent contractions (good!) it also made the pain of back labor more intense (arg!!). just after 10am, i decided a trip to the toilet was a good idea, so i peeled myself off my chair and headed that way past the business of kitchen tub-filling. as soon as i sat down on the toilet, a contraction started, and then as soon as i flushed the toilet, with a POP and GUSH, my water broke. i tried to look down to see the fluid, but it was basically world’s worst timing—i couldn’t tell whether the waters were clear (more on that later) as they flushed away mingled with loads of bloody show. damnit.
instantly with my water breaking (“spontaneous rupture of membranes” in medical parlance), i felt a flood of relief. back pain vanished for the next contraction as it had once in the chair, and i imagined that bean had shifted some when the cushion of water between her head and my cervix had let go. softness and strength returned, and i was (very briefly) in the driver’s seat again. in that moment, which felt so much like renewed positivity, i remembered a former client of mine who had let me know before labor that she couldn’t tolerate the feeling of a “bulging bag of waters” as it’s called and would want me to break her water for her at a certain point in her labor to provide her relief. i understood then what she meant. so much relief.
since my water had broken, acadia came into the bathroom to listen to bean with the doppler (we do this to rule out something called a cord prolapse, where the cord slips out ahead of the baby) and bean sounded great: heart chugging along in the normal range—no prolapse. i wiped to try to get a sense of whether the still-leaking fluid was clear or whether there was any meconium (baby’s first poop, which they pass in utero either when stressed or, much more frequently, when healthy but mature or “overdue”). what i got loads of obscuring bloody show, and there was some brown tinge, but old blood can be brown (right?), so it didn’t register. or maybe i just hoped it wasn’t meconium.
i’m reminded as i write this of one of my midwifery teachers who used to tell us “hope is not a management strategy—never forget that.” and yet, i hoped.
after rupture, i was quickly heartbroken as the reprieve from superfluous pain ended and the back labor came rushing back again full force. more and more, it was a building sense of “this is not right—this is not what it’s supposed to be like”, and that attitude/perception shift made coping more difficult. i remember thinking that i didn’t want to call the birth photographer yet because this part was so hard and ugly that it wouldn’t be what I wanted to remember. surely, i thought, it would change as labor wore on. those would be the parts i’d want to remember. I’d call the photographer when that shift happened, i decided.
after i eventually got out of the bathroom, the tub was ready, and i shucked clothes and got in. one leg over, the other leg over, then body in—i was overcome with SO MUCH RELIEF sinking into the hot water. i had set up the midwives’ aquadoula, a huge firm-sided tub with heaters that would keep the hot water hot. as i melted into the softening invitation of the water, my fixation points became the names of babies born in that tub, permanent-markered on the blue tub walls under the clear plastic disposable liner. so many humans had entered the world in that container, and bean was about to join their ranks.
the place i’d chosen for the tub was the sunny breakfast nook off the kitchen directly across from a home altar covered in magic bits and bobs shared with me at my blessingway the month before. candles, affirmation cards, beads, smudge, stones, statuary—i’d set it all up with the intention of having an intensely magical focus spot to dwell on when the going got tough. there were new items from loved ones and lineage pieces loaned out and passed around to laboring folks in community; it was (and still is today) a powerful testament to the transformative magic of birth.
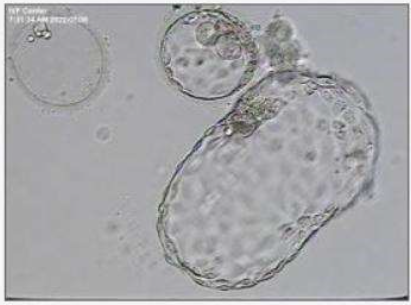
reclined in the tub, as had happened with the sterile water papules, i felt the scary sensation of sacral pain start to break through the relief afforded by the water. i kept moving, exploring contractions in seated, reclined, and kneeling positions, and i continued to try to will bean to move. I massaged my belly gently between contractions, urging the knobby knees below my ribcage around the side towards my back to hopefully be replaced by bean’s sweet, pointy frog-bum, but nothing budged. as i floated there, I noticed some odd light golden-brown flecks appear in the tub water…
if there’s one other thing that’s true about birth, it’s that LOTS of things come out of a body throughout the process, and waterbirth seems to amplify the obviousness of this fact. little swirls of blood, bits or blobs of mucus plug (the jellyfish-esque substance that protects the opening of the cervix and that lets go as the cervix opens), mini-confetti bits of white as waterlogged skin peels and sheds as you soak, and eventually, to absolutely everyone but the midwives’ horror, there’s usually also poop, which is why birth kits contain aquarium nets. this doesn’t happen until pushing though, because in a battle for space between a baby’s head and your poop, a baby’s head will aways win!
but back to the flecks… my eyes fixed on just two or three of them swirling near the surface, tiny and unassuming, but my midwife brain couldn’t reconcile what, besides evidence of meconium, they could be. maybe, hoped my heart, they were just some debris that had entered the tub stuck to the bottoms of my feet (but again, you know what they say about hope…)
once water breaks, it stays broken and generally continues to leak because baby keeps making more (amniotic fluid is dilute fetal urine—now that’s a thing you know!). whatever’s in the fluid becomes evident as more and more of it leaks out, and meconium, baby’s first bowel movement, is something you might see. If someone is early in their gestation, say like, 37 weeks, it’s more likely to mean a stressed baby who has let fly with poop in response to whatever is going on. with 41 and 42 weekers (my category), it’s more likely just a sign of fetal maturity—a system that’s ready to work has, well, started working, diaper or no.
it’s not nearly as gross as it sounds—it’s not at all poop in the adult human sense. meconium, or “mec”, is made up mostly of things that are shed and then swallowed by the baby in utero: epithelial cells (shed skin), lanugo (fuzzy baby hairs that you might see on a preemie but that mostly fall out in utero before birth), and vernix (the creamy white substance you see on some babies when they’re born), as well as bile produced by the baby’s liver, which gives it the distinct green/brown color. there isn’t the robust profile of microorganisms in mec like there is in adult poop, so it’s just sticky and odorless. if you’ve changed a new-new baby’s first few brownie batter diapers, you’ve met meconium.
after a good long soak in the tub, i decided to hop out and hit the bathroom again to see if i could figure out what the sitch was with my amniotic fluid. contractions were still coming every four minutes or so, and somehow, the back labor always seemed juuuust a little bit worse than before. i was starting to need specific positions for coping, and upright forward leaning was about the only thing that gave me any relief. after I peed, i wiped and checked the toilet paper—lots of bloody show (yay!) and a distinct golden brown schmear that could only have meant one thing: bean had pooped the bed.
goddamnit.
the worry with mec is that, since babies do practice breathing with amniotic fluid, they’ll inhale it, which can cause chemical irritation and/or physical obstruction within a baby’s lungs, subsequently harming their ability to take and sustain breaths once they’re born. meconium aspiration syndrome (MAS) is uncommon in low risk pregnancies, but it’s the worry any time there are mec-stained fluids. midwifery management depends largely on where a person is in labor. if there’s mec in the fluid and the birth is imminent, you prepare for possible resuscitation, get the baby born, and then monitor the heck out of them. if there’s mec and the birth is likely far off, you consider transport to the hospital where baby will have access to more respiratory support resources. sometimes you don’t know there’s meconium until the birth if the water doesn’t break until baby makes an entrance. almost always, no matter the timeline, meconium babies are born without issue—it’s more about being proactive just in case.
since we needed more info, i asked acadia to check me to see where I was in terms of dilation so that we could make a plan. “8! 8! 8!” I was hoping, based on the intensity of sensation and the frequency and duration of the contractions. vaginal exams are never terribly comfortable in labor, but i was curious to know, and really, we needed to know for best decision making. we went back to the bedroom and timed the check between contractions so that i could lay on my back without the incredible stabbing back labor pain.
she checked.
i was 4.
oof. 4 centimeters. under other circumstances, this would be fine, dandy, and so incredibly normal, especially for a first-time laboring person. it was noon and i’d been in early labor for around 15 hours and having serious, strong, regular contractions for around 6 hours, so 4 centimeters was a great result of all that good hard work. what happened next though changed the terms and the timeline.
when acadia finished the exam and removed her gloved hand, out came fingers coated in the thickest most obvious meconium i’d ever seen in my time as a midwife. SIGH. we knew what was next, and while not at all alien or scary to me, it was very different from my original plan. bean sounded great and was tolerating labor so incredibly well, but she was telling us we needed to be somewhere other than home for this birth. (and when babies talk, you always, ALWAYS listen.)
we finished up the exam and came into the kitchen and both in measured and calm midwife voices (it’s ingrained—you can’t help it) shared with stephen our thought that home was no longer the safest place to be. as i think back now, i’m trying to recapture how i felt in the moment. i know there was disappointment, but it wasn’t crushing, because i knew it was a good solid decision. bean’s and my wellbeing was top priority over giving birth at home, so i think it was more of an “uhg, damnit” than a soul crusher.
the next decision we had to make was where to go. my top choice would normally be memorial, the smaller local hospital here in the mount washington valley. i’ve transported and doula-ed there so many times, and i know, trust, and appreciate the providers and care staff there. if we’d been going in for a “me” issue, that’s where we’d go, but we weren’t going for a me issue, and memorial doesn’t have a nicu. a big issue with bean could mean being sent by the team at memorial on a very long ambulance ride or very expensive flight to our big tertiary care hospital in portland. as much as i wanted to avoid a 75-minute drive to the city (more on that nightmare in a bit), loads of provider changes, and a sea of unfamiliar faces, i knew and was able to vocalize with comfort and clarity that maine med was the better choice for bean, and since bean was why we were going, that’s where we’d go.
the next half hour or so was a familiar dance that i’ve done may times as a midwife but never as a laboring person. acadia called the hospital, gave report, and faxed in my records, i grabbed a bag already half-packed for memorial as a just-in-case and quickly realized that i’d need a different array of things with me if stephen wasn’t able to just pop home as needed. packing for a birth 75 minutes away meant packing for the long haul, which in case of a possible abdominal birth (“out the sunroof”, one of my clients says) could mean three days or more.
i puttered around grabbing clothes and a few extra toiletries—still contracting, still mentally mitigating the stabbing back pain—and in my shuffling about, my sprawling kitchen altar caught my eye. all that power and all of those special things that i wouldn’t be able to take with me. it felt like planning a party that i was about to miss. all that energy and intention that i wanted near me, and i was going to be leaving it behind. i ran my eyes across the items and grabbed two things that called to me as helpful, mobile, and accessible: a bean-shaped and palm-sized polished carnelian (a stone that had caught my eye all pregnancy for some reason, so fortuitous as a birthingway gift from a bosom bud), and an electric candle with an origami star wrapped around it and the word “trust” written on it (no real candles allowed in the hospital). i dropped the items in my bag and zipped it up. essence-of-altar officially in tow.
the ride to portland was something that i think both stephen and i deserve medals and an ice cream for. for stephen, it meant focusing on the road, on traffic, and on the nav while his person writhed in agony next to him (he did beautifully), and for me, it meant feeling with every ounce of my being (but mostly with my low back) exactly how long 75 minutes is. sitting was excruciating and triggered longer and more frequent contractions, and the pressure of the car seat on my tailbone ramped the back labor up a notch. at this point, i would have rated the sacral pain a 9/10. (cue voice of morgan freeman: “her pain was, in fact, not a nine, but a three on a scale that she could not yet fathom…”)
once we were solidly enroute, i figured out that because the infant car seat was installed behind me, i couldn’t lay my seat back (my body was screaming for me to do this); i had to sit bolt upright. as contractions and the accompanying ice pick hammering into my sacrum raged on, i contorted myself into as flat a position as i could, with legs outstretched and feet pressing into the upper back wall of the floorboard, head and left shoulder leaned into the middle space between seats, left elbow jammed against the arm rest. my new visual fixation became the pattern in stephen’s car headliner—i got lost in it like i had in the pattern of the chair.
“relaaaaaaaaxrelaxrelax”, i panted during contractions (mr. freeman: “she did not, in fact, relax…”)
“one more done. you never have to do that contraction again,“ i thought when it was done. i was starting to despise what felt like meaningless midwifery drivel served up as self-talk—i’d said that to so many people before, and i wanted nothing more than to tell myself to shut the fuck up saying it now.
every so many eternities, i’d glance up at the car clock—each time i did, fewer than 5 minutes had passed. the ice pick sensation teetered mightily close to the feeling of a bone being wrenched in half. the tight quarters meant i had to work hard to keep panic at bay. one way i did that was by keeping a bit of my midwife brain turned on. i’d brought the doppler and gel with me to continue to listen to bean every 20 minutes or so. i was in agony; bean was bopping along at a blissfully unbothered 140 beats per minute. together in a body, but worlds apart in the experience.
***
early in the afternoon, we arrived at the hospital, wound our way through the parking deck, met back up with acadia, and started the long walk to ob triage. it was a path I’d taken SO many times before with other people, but i’d never really noticed just how long it was. i was contracting like crazy, and every few yards we’d have to stop so that i could lean on stephen, bury my face in his shoulder, sway my aching hips back and forth, and breathe aggressively through a contraction. i humored the idea of a wheelchair, but i really couldn’t fathom more sitting.
parking deck. elevator. flyway. long hallway past information. another long hallway to the check in. waiting in line at check in. waiting for verification from ob. another elevator. another long hallway. (who on EARTH designed this floor plan??)
once we got up to ob triage, i was greeted by a fantastic duo of nurses who would be part of my team until shift change that night at 7. their eyes and voices were warm and inviting. “we know this was not part of your plan, but we’re happy to be able to take care of you and will do everything we can to keep the birth as close to the original plan as possible.” (thankfully gone are the days, at that hospital anyway, of being received as a pariah for having planned a home birth). i also met one of the obs, and though i don’t remember his name through the haze of labor, i remember thinking i wished he wasn’t going off shift at 7. he had great energy.
the team’s first task was full vitals on me and bean. my blood pressure had been high for the last week, but it wasn’t high enough to make anyone at the hospital bat an eyelash. 150s/90s. as a 110/70 gal, it had my panties in a wad but only triggered watchfulness from the team. bean had a good long listen via non-stress test (nst) which meant putting a stretchy belly band on me and tucking two wireless monitors into the band—one to track my contractions and one to track bean’s heart rate. bean was (and continued for the rest of the labor to be) just peachy.
i spent a great deal of my time (maybe two hours?) in ob triage forward-leaning over the bed which a nurse had raised to hip-high. i kept my right leg thrust out behind me, lifting it slightly with contractions to try to take the pressure of bean’s noggin off the inside of my sacrum. i noticed that everything that i did was protective and preventative—i couldn’t really lean in and let go because the additional pain above and beyond contractions was too bad, a roadblock to the positive no-way-out-but-through feedback system of labor.
in ob triage, that supplemental pain transitioned fully to bone-break. i felt like someone was cracking my sacrum in half for two out of every four minutes on repeat. oddly enough, one form of pain relief turned out to be the multiple attempts of the long-suffering nursing staff to place an iv. fifth time’s the charm for a hard stick like me, turns out, but the pain from prolonged fishing with an 18-gauge iv cath registered as relief compared to back labor—it was an odd and interesting short circuit! i remember thinking “you’ll need a vein-finder and you should call a picc nurse,” but i don’t know if those words actually made it out of my mouth. i’m guessing not since the massive amount of bruising made me look like i’d been in a car accident. i can’t blame them though—i’m a REALLY hard stick.
it took about two hours for a birthing suite room to open up (good day to have a baby I guess!), and we made the very long walk from ob triage to labor and delivery. i stopped over and over along the way to have contractions, leaning hard on stephen who held me tight and modeled deep, slow breathing. every nurse we passed gave kind and knowing smiles or soft words of encouragement. there was such an attitude of welcome about the place, and for that I was grateful.
walking through the door of room 2724 was like entering the uncanny valley—i’ve clocked SO many hours in those rooms as a doula. in the room the lights were low, there were battery powered candles everywhere, there was soft music playing, and there were my two trusty nurses. they helped me get straight into the tub, for which i had high hopes, but it turned out not to be deep enough for any sort of tailbone-sparing weightlessness. i mostly felt like a turtle on its back in too-shallow water. i guess they have it that way for safety reasons, and i imagine a smaller body might have a different experience of it. the situation was also complicated by my iv port—i couldn’t submerge one of my hands, so repositioning was suuuuuper awkward.
the last straw for the tub was when, just after signing consent forms for an admin dude who i suppose has seen just about everything, i started to feel sick and then vomited almost a quart of lemon-lime liquid iv into a hospital water jug. puking while reclined and one-handed in a shallow, not-hot-enough tub and immobilized with contractions—1/10, do not recommend.
fun side note: when you’re in labor, any notion of modesty tends to go out the window. shucking clothes to get in the tub would be the last time i’d wear anything besides a belly band and fetal monitors until well after bean was born. it seems funny looking back, thinking about wandering around naked and howling in a sea of shift-change strangers, but in the moment, laboring folks give zero fucks—to be certain, i did not.
***
at 6:30pm, shortly after i got out of the tub, the incoming doc came to introduce herself, and asked if I’d be ok with a check, since it had been six and a half hours since my last vaginal exam. navigating cervical checks when contractions are roaring can be tough, but i really needed some good news, so i said yes.
a quick check later I got the news: 6 centimeters (dilation of cervix), 70% effaced (percent thinness of cervix), and -2 station (the lowest part of bean’s head was 2 cm above my ischial spines—google it for a visual reference). even though the progress was super reasonable, i was (wet, nude, tired, and) crestfallen to only just now technically be entering “active” labor. for first babies, this means there’s likely *quite* a while to go. it also means that the most intense part of labor, transition, is still ahead, and i wasn’t sure how that uptick would impact the back pain.
for the first time, as the sacral pain somehow continued to intensify, and as half a day or more of additional labor loomed large, i started thinking about pain relief. i knew for sure that i wasn’t interested in opiates or other injectables—i’ve mostly seen people hate the wine-drunk feeling of still experiencing pain but having less mental capacity to cope—so i thought I’d give nitrous oxide a try. an incredibly short-duration analgesic, nitrous is something familiar to most folks who have had any dental work done in the past. in labor and delivery, it’s administered intermittently rather than continuously via a mask that the laboring person draws breath from and then exhales into. the person is responsible for holding the mask to their face (no one else can hold it for them), and the system scavenges exhaled nitrous to prevent everyone in the room from becoming lightheaded.
the plasticky smell and soft cushion of the mask sealed against my face and the intense valve rattle on inhale are incredibly vivid sensory memories of the evening for me. in the beginning, the nitrous provided some relief—i would start to draw strongly on the mask with slow deep breaths as soon as a contraction started. the rattle sound let me know i had the good seal necessary for the delivery system to work. after an hour or so, the effect began to wear off, but the slow deep breaths into the mask had become my new ritual. I think it was helpful even just to center and slow my breathing. the pain was still present, but the nitrous had the blessed effect for a while of making me care just a little bit less, and the feeling dissipated the moment i let go and breathed room air again.
cue my team of super nurses! (i feel so bad that everyone’s names and faces melted away in the blur of labor—your thinking brain really does go offline!). they got me and my nitrous cart situated into a new position—up on the bed, hands and knees, forward leaning over an inflatable birth stool (the cub—they rock!). one of the nurses positioned herself behind me and started some incredible deep tissue massage and myofascial release work on the deep muscles and connective tissue of my bum and thighs.
“holy wow, lady,” she said. “this is all kinds of knotted up on the right side!”
i remember thinking this was literally the only bad thing about having a hiker’s body: glutes, thighs, and a pelvic floor of steel can be less than conducive to letting babies pass by, and my right side was definitely my knotted up power-lifter.
after the massage, the nurse grabbed a sheet, cupped it around my bum, and started sifting back and forth, asking the musculature to let go and bean to please, please, please make the turn to back-in-front. she’d sift between contractions; i’d hungrily draw nitrous when the pain hit. looking back, that combo might have provided the most relief of anything we tried. i absolutely melted forward into the cub and let my whole body go for the very first time all labor. i think acadia also took a turn with massage and sifting, and someone was rubbing my feet, but i had my consciousness turned half off and my face buried in the smooth, turquoise birth stool, so i don’t have a great sense of who was doing what.
in my time in that position, i had one more contraction that was “just a labor contraction”. it felt incredible—powerful, intense, and not at all like a sledgehammer to my low back. the feeling was a relief but made me sad—this was what I’d signed up for, this was the sensation i’d been ready for, and it wasn’t what I got. labors though, don’t really care what you’ve signed up for, and i knew that.
***
shift change saw my proactive nursing team leave and a kind but less involved night nurse come on. the minutes passed, measured in pain that i increasingly couldn’t cope with. i remember the room being dark and, besides the mediative and repetitive music and intermittent rattle of breath drawn from the nitrous mask, quiet. i’d sunk deeper and deeper into an asymmetrically melted forward lean over the birth stool as the back labor roared on.
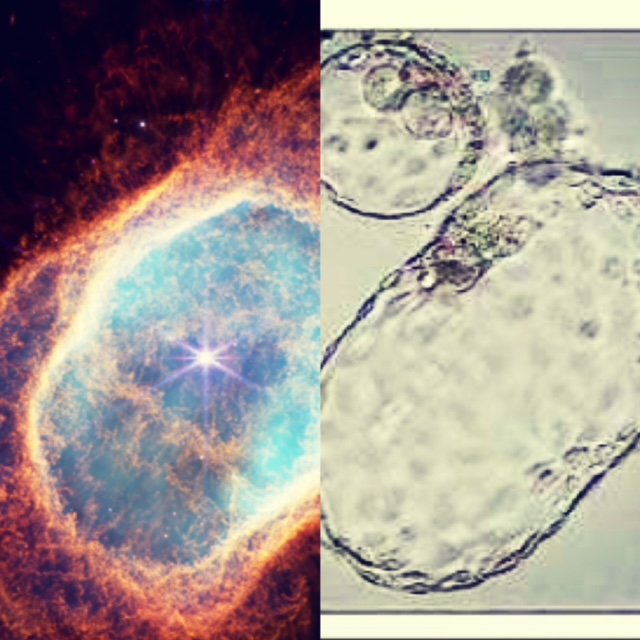
around 8pm, i knew i needed a change. i sat up onto my knees quickly, trying not to bring on a contraction, and in doing, peel-abraded my left arm which had become stuck to the plastic of the inflatable stool. i’d have an intense stippled bruise in that spot the next morning, like the colorized image of a nebula.
i remember looking at acadia and stephen in that moment and vocalizing what i’d been trying to define for myself through the fog of the last hour. what i was feeling had transitioned out of the realm of pain: it had become suffering.
“i need an epidural. i don’t mean it, but i need to say it and try it on.”
i’d coached dozens of doula clients through that same moment. say it. try it on. see if it feels real, and put it back in your pocket if it doesn’t. i wasn’t sure that it did, and in that moment, it still felt a lot like failing to think it. in response, acadia did what every good doula does when they know their person really doesn’t want an epidural, which is to stall and redirect. she suggested we try the shower instead and see if that provided any relief—we still had tricks to try before the epidural.
the shower had a fold-down seat in it, and i spent a good deal of time in the small stall with my back to the wall, facing out into the bathroom, left knee and both hands on the seat, right foot planted on the floor of the shower. the hot water was directed to my low back but poured over most of me. i have some vivid memories of white knuckling the wet, white, hard plastic seat, my shoulder blades reaching up like on a prowling lion, water splashing out into the bathroom (and onto stephen) faster than the nurse could mop it up with towels (another bathroom plumbing design flaw for the sake of safety, she acknowledged).
i was there for quite a while, and when the shower eventually stopped working (or maybe when i fatigued of hearing my own loud vocalizations in such a bright, echoey room), i decided that what i desperately needed was rest, and i had a super clear image of how i’d get it. i asked the nurse for a mat, the kind they put on the delivery beds to make them less awful, and a sheet, and i was going to work through the miles circuit once more on the floor. i figured in deep knee-chest and extended side-lying positions, i could both rest and encourage bean to turn.
(real time author note: new day, new clothes, similarly in need of a shower, but bean gave us a luxurious 7 hours of sleep last night! back at the kitchen table while she plays on an activity mat beside me, reflecting on how the timeline of writing (and everything else) is so dramatically different when you measure your day out in 15-minute increments. i read yesterday that having a newborn adds over 300 tasks to your day. Truth. i’m noticing more clarity as i write, so i think the iron infusions are working—but more on that later.)
i dried off from the shower in between contractions and settled into my new spot, desperately trying to rest. i hadn’t had anything appreciable to eat in 12+ hours, and i was in awe (and horror) that the intensity of the back labor pain seemed to increase despite, i thought, hitting “10” on the pain scale multiple times before. acadia spoon fed me greek yogurt and i kept sipping on lemon-lime liquid iv. i wound up sinking into a messy, sprawled, side-lie with my left knee up; my wettish bun had hit the “indistinguishable” hairstyle phase—i’m sure it was a positively primal sight.
i wasn’t totally aware in the moment, but what i was doing in the floor, in addition to trying to recharge, was *avoiding* contractions; i’d stopped giving in on any level to labor. because of bean’s position, any time i or bean moved, it would also trigger a contraction that began with the excruciating back pain. staying still meant fewer contractions and a bit of a break, but it also meant less productive labor. as i rested, my pattern spaced out to about every 6 minutes or so, and i drew hard on the nitrous with each bout of agonizing pain. at that point, i felt zero pain-relieving effects from it, but the ritual of deep breathing into the mask had become important. i was trying so hard to be ok, and in the process i was absolutely saying “no” to labor.
while i melted and avoided, stephen took the opportunity to lie down on the couch beside my makeshift pallet and catch some much-needed sleep. acadia rested as well as a midwife ever does, which usually means closed eyes but a deep awareness of every sound—contractions, upticks in intensity, the beep-beep-beep of the fetal heart tones, and in this case I’m sure the deep rattle of my draws on the nitrous. it all felt like years, but it was maybe an hour and a half of molasses sub-consciousness on the floor of my hospital room.
***
at a quarter to 11, my doc popped in to check on us and help plan next steps. she let me know that contractions had spaced, and she asked if a vaginal exam would be ok since around 4 hours had passed since the last check. thinking back, i can’t remember if she checked me there on the floor or if i managed to get up on the bed. my brain says floor, but that time is all a pretty intense fog of dimly lit attempts to will my physical body to disappear.
she checked…and i was crushed. 4 hours later, i was still at 6cm, still 70% effaced, and still -2 station. i couldn’t fathom how the intensity of the last 4 hours had brought about no progress. to make matters a little worse, in addition to still being posterior, bean had, attempting to navigate a tough situation, cocked her head to the side, so that rather than leading with the symmetrical roundness of her occiput, she led with the bony protusion of her left parietal bone into my pelvis. (google “litzmann obliquity” for a visual). she was developing a little bit of caput, or swelling, on her noggin where it pressed into my cervix (totally fine, but often an indication of very slow going with lots of sustained pressure in one place).
I wanted to escape out of my skin an into a different plane of existence. i was able to identify in that moment that my avoidance of contractions wasn’t sustainable, and i knew what the doc would likely (and in my case helpfully) suggest as a solution:
“so we’re not seeing a lot of progress here, and your contractions are spacing out. At this point, I think my recommendation would be that we start a little pitocin to see if we can coax things back into a more active pattern and get baby moving for you.”
in that moment, i knew three things:
contractions that were longer, stronger, and closer together were my only way through, and pitocin would get me there, but…
i couldn’t fathom intentionally pharmaceutically intensify something that already felt physically, mentally, emotionally, and spiritually untenable, and…
i didn’t want an epidural (and the emergent cascade they can cause), but that would make way for my only imaginable “yes” to pitocin.
“i need to talk to my team,” i told the doc, amazed that something so rational had come out of my mouth in that moment. she agreed “absolutely of course” and gave us the room. the three of us had the talk. none of these were things that i wanted, all of them were things that i as a person and midwife knew would help me, and there was grief in the fact that none of this was at all part of my vision for myself. i’d been there so many times with clients, and in the moment, i was telling myself (and it’s absolutely true), that there’s a time and place for interventions, and part of the challenge is recognizing when they’re appropriate and might actually help. and as with so many of my clients, i was noticing that the idea of an epidural felt like a failure—i noticed that feeling, said hi to it, welcomed it into the space, and then challenged its veracity.
the honest truth was that it wasn’t a failure—it was a route out of suffering and hopefully a gateway to having bean in my arms. something in the interplay between bean’s body and mine was holding her in a position that was causing a real mess, and the combination of rest for me and complete relaxation of my pelvic floor would hopefully shift the situation in a big way. it was also valid and ok that it felt for just a moment like failing. both truths can exist.
we called the doc back in and shared thoughts. i would consent to pitocin augmentation on a “low and slow” setting, but only if i had an epidural on board. i couldn’t see how i could stay still and in position for epidural placement, but i knew I’d just have to figure it out.
half an hour later, the anesthesiology duo came to my room. in that short period of time, i’d transitioned from the feeling of failure to a sort of euphoria at the idea of relief from the cracked-in-half sacrum nightmare. i was excited for an epidural. i knew it was the right choice and a good use of the tool. i was ready.
“so before we get started,” the anesthesiologist said, coming near, “i want to let you know that an epidural, unfortunately, is very unlikely to do anything to change the sensation of back labor. it will take away the abdominal contraction feeling, but not the back labor, i’m afraid.”
cue flood of utter despair-panic.
i’d come to terms with an intervention that i definitely didn’t want, and now i was hearing that it most likely wouldn’t work. i sunk into stephen’s arms as we stood there, and i could see and feel acadia’s empathic response to me likely losing my one lifeline. i felt completely defeated and like there was no way out. i thought for a moment: so my two roads here are pitocin and stronger labor for 12+ more hours but no pain relief, or decline the pit and likely wind up with a section when the continued labor and lack of progress started to stress bean.
…or there was always the third option of trying the epidural anyway. if it worked, which sounded unlikely, it would be my way forward. if it didn’t, i could be completely immobilized in bed, still feeling back labor but completely unable to move my lower body as part of coping and as a strategy for moving bean. looking back, it feels nuts to have taken the risk, but everything in my body was saying to do the epidural anyway. try it. just try it and see. do iiiiiiiiit.
so we did.
epidural anesthesia involves introducing pain relieving medication into the “epidural” (above the dura mater) space in the spinal column. it’s like getting an iv in your spine in that a needle wrapped in a soft, flexible catheter is introduced into the body, and then the needle is backed out and only the soft catheter remains as an in/out body port. for the anesthesiologist to place the catheter, you have to sit on a raised bed, feet dangling off the edge, and curl forward like a shrimp, expanding the spaces between vertebrae for safe placement—completely still—while in raging labor. if you haven’t given birth before, imagine that every few minutes you’re have aggressively uncontrollable diarrhea accompanied by intense abdominal pain and your body pushes down and out no matter what you do. now add an ice pick in your sacrum. now try to stay still while someone inserts a needle into your spine as you’re trying not to let fly.
funtimes. totes doable.
the anesthesiologist asked if i had scoliosis. “mild,” i said, “and degenerative disc disease…oh and a 6th lumbar vertebra.” which discs had ddd? i couldn’t remember. i managed to get into place on the bed and somehow will my entire body still during contractions. in that position, i developed another difficulty: an early urge to push. typically, an urge to push your baby out (which feels like “I’m going to poop—NOW” on steroids) hits sometime after you’re fully dilated and baby has begun to move down, pressing on the same rectal nerve involved with actually needing to poop. bean’s position with noggin digging into my sacrum was causing that to happen early. all you can do in those situations is “blow it away” by breathing like you’re blowing out candles on a birthday cake. it all feels a lot like realizing in 5 o’clock traffic that you’ve got food poisoning and the poop is coming whether you’re at home or in your car (margaret cho has a stellar standup routine about this involving too many persimmons and madonna’s song “holiday”).
leaning forward in my torturous shrimp curl, i felt the burning “pop” of the epidural needle into the numbed skin over my spine, then there was some fiddling around, and then i felt the needle come back out. apparently the ddd affected the space the anesthesiologist had gone for, narrowing the gap between my lumbar vertebrae. as the contractions rolled on, she let me know that she’d have to try again higher. i felt the same set of sensations further up my back, and then there was success. the needle was withdrawn, the catheter left behind, a bolus of numbing meds injected, and then the long tail of the soft catheter taped up my back and onto my shoulder. a titrated amount of medication would continue to be introduced through the catheter until the epidural was turned off or removed.
then I settled in to wait, hoping (the worst management strategy) that by some magic, the back labor would disappear with the epidural despite what the anesthesiologist had warned. i rolled onto my back to help the medication settle evenly on both sides of my spine. i dreaded the first contraction i’d have in that position, i dreaded losing sensation in my legs, and i dreaded the possibility of being immobilized and still in pain. dread and wait.
the nurse was fiddling around taking vitals, positioning my pillows, and all of the rest when a few minutes later i felt it—intense benign pressure in my pelvic floor and a tightening of my belly under my hands. completely. devoid. of. pain. just pressure. no pain. nada. nothing. complete relief. back labor… gone. i wanted to cry. i don’t remember if i actually did. the contrast was so stark, and i felt like i was waking up to hopeful clear-headedness out of a fog of hopeless pain.
“did I just have a contraction?” i asked, completely astonished. the nurse looked up at the monitor noted the jagged little hill on my graph and said “yep!”.
i’m not sure whether that moment or bean’s actual birth would register as more relieving. i’ll call them a tie. if ivf was the best decision i ever made, an epidural during back labor was the second best. i know it sounds odd, but there was also a tiny moment of grief over not being able to experience my labor contractions, but if it meant turning off the sacral pain, i’d happily make the trade.
(real time author note: this is at least my fourth day of writing—i’ve lost count. back at the kitchen table, clean, fed, done with laundry, just figured out cloth diapering—all in all an insanely productive day with a newborn. getting better at this!)
i felt like i was aware of the entirety of my surroundings and of the passage of time for the first time since mid-morning. my toes tingled and my legs were a bit heavy, but i still had full range of motion and strength as well as a great deal of limb sensation. i wondered if that would go away (it didn’t!). even though i managed near full mobility with the epidural, it wasn’t safe for me to try to walk around, so the nurse straight cathed me to empty my bladder, a procedure i experienced without discomfort (yay, small favors!). then she hooked the pitocin drip up to my iv port, set the infusion pump to 2, tucked me in, turned the lights back down, and left me to get some rest.
i stayed on my back under warm blankets because it was, for the first time all labor, comfortable to do so, and with stephen once again sleeping on the couch and acadia midwife-napping on the mat in the corner by the birth tub, i drifted off into a completely and totally blissed-out sleep. all i felt was painless, powerful pressure in my pelvic floor every 3-4 minutes as my body continued to contract. bean chugged along in a healthy range, just loving life.
we’d made it through the dark night.
may 1st, a monday (and a flooding-rainy beltane)
i woke up from my short but deep bliss-sleep around 2:30am to the sound of the door opening. I was in the same position i’d fallen asleep in, and i felt complete renewal. the doc and nurse came in, and the doc shared that, if it was ok with me, she’d like to recheck my cervix to see what, if anything, the pitocin and epidural had accomplished in the last two hours. i agreed then reached my hands down instinctively to give my belly a rub and a pat. in doing, i noticed what felt like an incredible gift: the long, hard curve of bean’s back on my front right side. if nothing else, she was no longer posterior. something in the complete melting relaxation of my body had made way for her to move.
i got into position on my own, with knees butterflied to the side, and the doc reached two gloved fingers towards bean’s noggin with pressure but no pain. (it’s always the longest wait as a provider tries to gather maximum information in one go.) i hoped she’d say 7—a clear sign of progress but thought that we’d be ok no matter what. all the while, stephen still slept and acadia “napped” attentively.
“well,” she said with a smile, “baby has come around to the front, the asynclitism has resolved, and you’re completely dilated—are you ready to push your baby out?”
BEAMING TRIUMPH. (And pretty intense disbelief.)
“wait, like… all the way? as in 4 centimeters in 2 hours?”
“yyyep!”
i did a quick check-in with my body sensations; i was pretty sure that I wasn’t noticing any involuntary pushing or bearing down, meaning that if i didn’t have an epidural, i’d be in the magical “rest and be thankful” phase that hospitals typically ignore but that midwives know often comes between transition and pushing, especially for first time laborers. when unmedicated, a person in this space seems to “wake up” from labor land, as i had when the epidural had kicked in. they go from closed-eyed animal brain shutdown of executive function to something closer to their ordinary selves. personality comes back online, speech returns, and folks often feel calm, relieved, and to an extent back in control. (subsequent births will often steamroll right past this phase into a quick push).
i asked if it would be possible, since bean hadn’t moved down yet far enough to trigger pushing, to do what’s called “laboring down”, meaning let my body keep going doing its thing without additional effort from me. the goal would be for my contractions to move bean down a few more centimeters toward the outside world so that i wouldn’t have to completely exhaust myself unnecessarily by wailing on pushes. i’d seen so many people in the hospital push for 3 or 4 hours with an epidural, and that seemed like such a waste of energy.
the doc said she’d chat with her team and make sure they were comfortable with that, and she was back in a flash to say yes and to ask if 30 minutes would be enough. it absolutely would not, i thought, but i knew that “30 minutes” in labor and delivery time likely meant an hour and a half as people got busy, so I said “yep”.
after we checked in about a few birth and immediate postpartum desires, she left, and i continued to rest without bothering to wake my team. they all needed sleep (or rest, at least) and there was no reason for anyone to spend my laboring down time awake. i looked around the dark, calm, quiet room and soaked it in, knowing that soon enough a cacophony of humans would pour in: nurses and my resident doc first to get me started pushing, and then a slew of other residents and students, an attending physician, more nurses, and the neonatal team for bean, a precaution since there was meconium in my fluid. controlled chaos.
and then sleep overtook me again.
eighty minutes later (ha!) i woke back up when the doc and nurse returned to get me pushing. i woke stephen up with the amazing and impossible news that i was fully dilated, and acadia popped up from her rest perch in the corner. when a first-time birthing person is about to start pushing, precisely no one is in a hurry, so things were calm and relaxed. i asked acadia to call taraé, my photographer, because birth was starting to feel for the first time like something i WOULD like to remember.
i started to experiment with pushing in a right side-lying position with my left leg up and supported. since i couldn’t feel the building sensation of a contraction, i relied on noticing an increase in pelvic pressure. there’s no point in pushing when your body isn’t involuntarily doing the same (that’s a recipe for exhaustion), so whenever i felt the pressure on my pelvic floor intensify, i lifted my leg and started to bear down. i didn’t have any interest in hospital style “purple pushing” where you hold your breath while someone counts out loud to 10, so i tried to take each contraction as an opportunity to get in 3 or so good decent pushes, with plenty of oxygenation in between.
it takes a minute to get your bearings pushing for the first time—figuring out where and how to send the energy down—but i got it pretty quickly. (pals and I say that large-bodied people always do because of our relatively massive core strength. carry around a bigger body, enjoy increased power!) i sent the energy down to my root chakra, curling around my belly and giving into a sensation uncannily like pooping when you’re really consitpated. “it’s like pooping but with a cuter result!” i tell clients. (and there’s almost always also poop, because as i mentioned earlier, in a battle between poop and a baby’s head…)
since pushing out a first baby is a game of hours and millimeters, we took our time, and i experimented with a number of different positions. after a couple of side-lying rotations, i decided to try, despite my epidural, to get up into a hands and knees position on the bed. to my surprise, i was highly mobile and easily able to do so once i figured out where and how to arrange the blood pressure cuff cord and iv tubes. in hands and knees, i found my power position: when a contraction would start, i would sit back into a low squat, like a modified child’s pose, and press bean’s bulk deep into my pelvis, and then when the contraction was over, i would relax back into hands and knees or a deep knee-chest position. i could tell this was moving bean down because of the increase in pressure in my vaginal canal and on my rectum—it felt like i was trying to poop a watermelon (which I suppose in a way I was). acadia gave me counter-pressure with a warm washcloth, which helped the “my butt might explode” feeling immensely.
as bean moved lower, the epidural became more and more obsolete, and the sensations of labor returned. since she’d turned into an optimal position and had gotten so much lower in my pelvis though, there were zero sensations of back labor—just strong and powerful contractions every 4 minutes that moved her down little by little. i have trouble describing the intensity of the pressure, but i LOVED pushing. it was powerful and effective—the opposite of a turtle on its back. it was pretty much exactly what i had expected it to be, and i was so grateful in that moment to have something feel “as advertised”.
as second stage (pushing) progressed and birth became more imminent, the room began to fill with folks who would comprise the birth team. it’s so very different from the atmosphere and approach in home birth—i think i had an attending and three resident physicians, at least two nurses, and a neonatal team of at least four whose credentials i didn’t know. as more people piled in the room, i decided to create a quiet little world of my own, slipping the cool wet washcloth that acadia had placed on my forehead down over my eyes—dark, calm intensity, mirroring bean’s last few minutes on the inside. i was settled on my back (who knew i’d like that?) and when i had a contraction, stephen would support my left leg up in an asymmetrical side-lie. i knew bean had gotten lower, so i reached down to feel, encountering the warm, wet, wrinkly scalp of a nearly earthside baby (like shar pei puppy skin).
i couldn’t believe we’d gotten here—from end-of-the-world to imminent beanification in just a few short hours.
“does she have any hair?” i asked.
“oh yes!” came the chorus. (so, it’s true what they say about heartburn.)
my absolute joy, the most intense, ecstatic joy I’ve ever experienced in my life, was holding my fingertips and eventually whole hand against the top of bean’s head while i pushed, gauging the productivity of my efforts by how much she moved with each effort, counting down the minutes ‘til we met. the doc asked if i wanted a mirror. i replied that i preferred to experience it through touch rather than through sight. i felt like i’d retreated deep into my animal body and didn’t need to open my eyes in order to “see”. when 3 or 4 centimeters of bean’s curly-headed scalp was visible (about the width of an oreo cookie), i asked stephen if he wanted to touch her. he said yes, and i guided his hand to her noggin, hard and fuzzy as an unripe peach (but one of those grapefruit-sized chilton county peaches, y’all). pure magic.
with each push, bean crept further forward, rocking under my pubic bone in a 3-steps-forward 2-steps-back dance that was so incredibly familiar to me. i felt the notorious “ring of fire” as the bulbocavernosus muscle and external structures of the vulva are stretched beyond imagination and beyond the reach of the epidural. when her head finally rocked under my pubic bone and stayed (crowning), i reached down and moved tissue gently around her head as i’d done for so many other first time birthing folks, and i asked for a warm washcloth so that i could apply warm counterpressure from above as the doc did so from below.
bean soldiered on with rock-solid heart tones—just a little normal dip at the end from all the pressure. when her head started to be born, i really gave it all i had, calling out “come on, bean, time to get oooooout!!” i asked the doc if i was pushing too hard or fast and she assured me that everything seemed incredibly controlled (wowza it didn’t feel that way!). with the push to end all pushes, bean’s head was born with a BUMP sensation, face looking toward the floor, in a flood of relieved pressure. she turned her head to match her shoulders (restitution), and then head and body together turned so that she faced my left thigh (external rotation; this realignment helps the shoulders to be born). most hospital births i’ve seen include providers rushing these steps to manually facilitate the birth of the shoulders and body, but that rushing can cause the problem it seeks to solve (stuck shoulders). per our earlier chat, the doc (mostly) let these things happen unbothered.
head born. i breathed. bean turned. body born. i breathed. it was such an incredibly odd sensation to feel her body leaving mine. she’d been so tightly packed in behind an abdominal wall that just wouldn’t give for such and long time, and then… out! woosh. relief. i pushed the washcloth off my eyes and reached down to see bean and grabbed at her hungrily, bringing her up to my belly. i was surrounded by bustling staff, but she, stephen, and i were the only to humans that existed in the world in that moment.
i pulled her warm wet body up onto mine (the HAIR, y’all!), and i could tell that she was a little bit stunned (babies often are). i welcomed her, kissed her, rubbed her back, and started to dry her off as she took a moment to really arrive into her body. and then I cried like a baby. she was trying to cry, but by a minute, her efforts were still a bit weak and her muscle tone was low (think a bit floppy rather than tightly spring-loaded like newborn limbs usually feel). i could tell she needed a bit more help (her 1-minute apgar was 6, with 0, 2, 2, 1, 1 scores), so the doc cut her cord (sooooooo much of her blood supply was still in that cord—folks, 60 seconds is not “delayed cord clamping”!) and they brought her over to the warmer. her 5-minute apgar was a 7 (1, 2, 2, 1, 1). Improving, improving.
i’d always imagined that if anyone needed to whisk my baby away, some animal anger would overtake me and I’d rage and gnash my teeth and snatch at my baby. it was perhaps my biggest birth phobia in case of transport (but has since been replaced by back labor). because stephen was able to accompany bean to the warmer though (and I’m sure the endorphins helped), i was completely calm. if she had one of us, i felt like she knew she was safe. if i could see him and he could see her, we were still connected. from my bed i listened as they deep-suctioned meconium out of her airway and belly and gave her a little breathing encouragement via CPAP. then there it was—a great big cry.
all i felt was relief and love.
***
over at the warmer, bean came around pretty quickly. “what’s her name?” i heard one of the nurses ask the team. “they’re calling her ‘bean’ for now” another said. “ruby!” I called out. “her name is ruby.” as soon as ruby was stable and happy, the nurse asked stephen if he wanted to diaper her for the first time, which he gladly (and I imagine gingerly) did, and then someone on the staff brought her to me. she was perfect and pink with purple hands and feet (which is normal), and bright, seeking eyes, and she was so warm and soft. her hair was a mess of blood and meconium, and she was the most beautiful thing i’d ever seen—my eyes and cheeks, stephen’s nose and mouth and (stephen and i both assessed separately) the spitting image of my brother jeff. she latched almost immediately, so i knew she’d really come around and would be just fine. I was completely blissed out.
***
one of the requests i’d made to my provider in our earlier chat was around management of the delivery of my placenta (the “third stage of labor”, with cervical dilation being first and pushing being second). in the hospital, providers tend toward something called “active management”, meaning they don’t wait for the body to complete the physiologic process of detaching and “birthing” the placenta; rather, they administer medication to stimulate uterine contractions and then often massage the belly and pull on the cord to hurry the process along. I was not at all interested in an interruption of the physiologic process without a good solid medical indication, so the team, despite a palpable tension and nervousness, “allowed” me 27 minutes to deliver my placenta. when it seemed like my placenta was ready to come, my provider helped guide it out (“easy, easy—soft and smooth—there are no bones in a placenta” I said to myself as if I were a midwifery client). my placenta came complete and without issue.
and then the bleeding started.
blood loss is a part of childbirth, plain and simple, and to the untrained eye even a normal amount of loss can look and feel intense. when the placenta detaches from the inside of the uterus, all of those little vessels that brought nourishing blood in close proximity to baby’s blood supply (the two aren’t mixed) will bleed at a fast rate until the uterus clamps down like a tourniquet. most folks lose at least a cup of blood during birth, and we don’t want folks to lose more than two (more precisely, 500ccs). for whatever reason, when my placenta delivered, that clamping didn’t happen, even with a contraction-stimulating pitocin iv on board.
i handed ruby, who was doing great, to stephen for some sweet skin-to-skin time, and the team shifted their focus to me. postpartum hemorrhage is a dangerous affair and is a very intense experience. the next twenty minutes were a flurry of action, in an attempt to diagnose what exactly was happening (you can bleed because of a tired uterus, a tear, part of the placenta left inside, or a clotting disorder) and to resolve the cause. the diagnosis was puzzling because i had no clotting disorders, my tear didn’t seem to involve any vessels, my placenta was complete, and the top part of my uterus was clamped down so hard that it felt like a grapefruit through my empty belly (which is a good thing).
as one provider started pumping me full of meds—pit, pit, misoprostol, txa, carboprost, carboprost—another took a speculum and pair of allis clamps and pulled my cervix toward my vaginal opening to check for cervical tears (as painful as it sounds).
nada concerning there.
bleeding, bleeding.
the only reasonable possibility left was that the lower part of my uterus was “atonic” meaning not contracting down along with the top part. (if you visualize a lightbulb, the wide part at the top is the upper uterine segment, the neck that narrows is the lower uterine segment, and the metal threading is the cervix.) the free bleeding there meant that the lower segment was filling with blood and that the pressure from the blood was keeping clamping from happening in a terrifying positive feedback system. doesn’t clamp down, bleeds, can’t clamp down because of blood clots, repeat.
what happened next registered as intensely emotionally and physically traumatic at the time and for the first few days postpartum, but i notice now as i write that i don’t have a particular visceral or emotional response when “going back there” (for which I’m thankful). in order to try to stop the bleeding, one of the doctors performed “internal bimanual compression”, which involved inserting a whole hand past the wrist into my vaginal canal (you know, the one that just pushed out a baby—the one with torn and traumatized tissue), making a fist, pressing up against the cervix and uterus, and then pressing down against that internal hand with an external hand on the belly.
i felt like i might lose consciousness.
that didn’t stop the bleeding, so the providers (3 of them) took turns doing “manual sweeps” to remove blood clots and check for retained tissue. this meant reaching all the way up into my uterus and “scooping” clots out by hand in an attempt to facilitate the muscular contraction that was needed to stop the blood.
over and over.
one then another. one then another.
i’ve never experienced anything so violating and excruciatingly painful in my life. intellectually, i knew that they were doing what they needed to do to stop my bleeding, but the soft animal of me just asked over and over and over for them to stop. they didn’t stop (because they couldn’t), but the real insult was that the whole time, none of them interacted with me like i was a human. no coaching me through the sensation. no “i’m sorry I know this is terrible, but we need you to stop bleeding”. i was just a body being acted upon emergently. i wasn’t acknowledged as a person.
the human element came (because of course it did) from acadia who was once again present with me like a midwife. she slipped the smooth, cool carnelian stone that i’d brought into my hand and coached me through breathing.
one reach in. searing pain. the misoprostol starts to make me shake violently.
one reach in. searing pain. the carboprost starts to make me nauseated.
over. and over. and over.
in the end i would find out that an (absolutely mortified) nurse had mistakenly turned off my epidural long ago but the providers seemed to be acting on the assumption that i still had an epidural and couldn’t feel pain from what they were doing. and while knowing wouldn’t have changed their very necessary management, it could have changed their tone and interaction with me. wouldn’t it have been amazing if they’d bothered to ask? I felt everything.
over the period of about 20 minutes (which felt like an eternity), none of the meds and none of the repeated uterine spelunking endeavors stopped my bleeding, so they eventually inserted a device called a jada, which is as intellectually fascinating as it was horrifying to experience (you know, without the epidural and all). the jada is a device that’s inserted into the uterus, and it uses suction to create a vacuum and clamp the uterus down around it. the insertion is no fun, but you don’t feel it once it’s in. the doc told me that we’d know whether it worked by the amount of blood collected by the suction—less than 500ccs (around 2 cups) and it “worked”; more than 500 with continued bleeding and it hadn’t.
in the case of the jada failing, the next step would be general anesthesia for a d&c, and if that didn’t work, he said, i’d have an emergency hysterectomy while under general. a picc nurse with an ultrasound machine came in and placed an auxiliary IV in my bicep (since ob triage had blown out my other locations) in preparation for the worst-case scenario (or I suppose all things considered, the second worst), then the team got the jada placed (excruciating) along with a foley catheter (heyyyyyy, no big deal).
at that point, i was exhausted, still lying prone under a warm white hospital blanket, with my feet up on stirrup pads, legs shaking violently from the misoprostol, hips aching from not having been able to move, smooth stone in my hand, eyes glued to my perfect curly-headed baby sleeping skin to skin on my husband’s chest. the tube from the jada and the tube from the cath were taped to my left leg and the sticky plastic stung like fire on my abraded undercarriage whenever i moved, like the stubbing burn of a hot playground slide on your thighs back when they used to be tall, metal, and hilariously dangerous.
“what’s my qbl?” I asked the doc. (you can always see the look of surprise when they first realize you’re a provider because they “skimmed” that part of your patient note).
“2300 so far” he said.
2300ccs. that’s 2.3 liters. that’s almost half of a pregnant person’s blood supply and the worst hemorrhage i’ve ever encountered as a provider. i could only lose 500ccs more if i wanted to keep my ute. check. on it.
alright body—time to listen to me. STOP BLEEDING.
and listen it did. the jada stayed in for several hours and maxed out at 330ccs. final qbl (quantitative blood loss) was 2,630ccs (holy shit). while the device did its job, the team checked out my perineum (which had been SO abused by that point). they disagreed as to whether i had a second- or third-degree tear but settled on a “3a”, meaning i’d torn down my vaginal floor, through my bulbocavernosus muscle, down the skin of my perineum, and just barely into the tissue capsule lining the anal sphincter but not into the muscle itself. i thanked the birth gods that it didn’t go further.
they numbed me up (finally!) and started the repair around 7am. when they were about halfway through, the side effects of the carboprost hit and i felt faint and incredibly nauseated. i let the doc team know, but they didn’t seem too motivated by the info. the nursing team ran for meds and acadia ran for a puke bag. the doctors were still engrossed in the repair (this was a teaching hospital, and one was narrating the repair to another) so i repeated “please stop for a second—i’m going to throw up”. the idea of heaving with a needle in my perineum skeeved me out big time.
they paused but didn’t help me reposition, and i tried to puke into a bag (unsuccessfully) by simply turning my head to the side since i was bound in place by the suturing situation. most of it wound up down my back, but thankfully it was just lemon-lime electrolyte drink. “man, the LAYERS of indignity,” i thought.
the antiemetic meds worked quickly, and the nursing team gave me a couple other things to counteract the gnarly side-effects of my antihemorrhagic meds. the miso shakes, unfortunately, continued for around the next 12 hours, giving me the appearance of someone perpetually cold.
after my repair, time becomes a bit of a blur because of exhaustion and blood loss. I was finally able to lay my legs flat and to hold and nurse ruby again with some assistance. i had labs drawn to start to assess the extent of damage from the hemorrhage, we saw the ped team who were mildly horrified that we were choosing oral rather than injectable vitamin k (and who gave me a bogus list of risk factors for vitamin k deficiency bleeding not at all reflective of the research, which was disappointing), and i had a blood transfusion of one unit of 0 positive blood (my profuse and humble thanks to my donor).
I was npo (nothing by mouth, including water) because of the threat of possibly needing emergency surgery, so i was parched and famished the whole time (like running a marathon and then not being able to eat after). the last meal i’d had had been almost 24 hours ago. one kind nurse prompted me to drink *all* the water (wink wink) that she’d brought with my last round of meds. best glass of water i’d ever had. a life-savingly kind friend and colleague brought coffee and food for my team and for me for when i was able to finally have it.
after several hours (and a great deal of relief that the bleeding had stopped), the jada was removed (like the worst tampon ever, the doc accurately described it) and i got to lose the foley cath. between the birth, the massively invasive repeated internal procedures, the cath, and the jada, my pelvic bowl felt completely wrecked and abused, like a basket with a burned-out bottom. i was starting to have intrusive memory flashes about the internal manual sweeps and my complete helplessness to stop them. it’s as close (thank the gods) as i can come to imagining what sexual assault must feel like after the fact. such a tough thing—it was absolutely necessary, but i felt absolutely scarred by it. both/and. the intermittent waves of panic that i would feel blessedly stopped a few days after i got home.
***
once i was stable and had been observed for the requisite number of hours, we were moved from the big labor and delivery room to a small mother/baby postpartum suite to spend the evening and night. i was in really bad shape from not being able to eat or drink anything after such a long birth and such a big blood loss. when i finally called the postpartum nurse that evening and begged to have my npo lifted since it had been almost 12 hours since my birth, she looked horrified—hadn’t anyone in labor and delivery told me that the NPO had been lifted hours ago? sigh.
with no more restrictions, i proceeded to down-the-hatch and entire coffee (without actually swallowing i’m pretty sure) and inhale pancakes from the food stash that had been brought to us by our team’s care angel, tiffany. when i finished, i ordered dinner. when i finished, i ate snacks. i. was. ravenous. and sore, and shaken, and relieved, and absolutely, positively, head over heels in love with the strawberry blonde (who knew??) squish in the bassinette next to me. 8 pounds 3 ounces, 21 inches long.
i *made* that. mind blowing!
besides some temporary, benign fast breathing (ttn), ruby didn’t have any other issues while there, and despite needing some help to get going, her vitals were strong and there were no lingering concerns from the meconium. i felt so bad for her as she kept trying so desperately to fall into the one big sleep newbs get after birth only to be awakened over and over by a nurse doing her rounds q 4h. it’s torture. the baby is FINE, please let her sleeeeeeeep! the madness we undertake for the sake of covered bases!
stephen got some sleep on the weird pleather sofa bed, and i settled in as best i could with a busted bottom on the uncomfortable postpartum hospital bed. the immediate postpartum after a hard first birth is a weird timeless space of extreme exhaustion paired with hypervigilance paired with full-body-hurt paired with the hypnotic urge to watch a baby like they were a riveting show. caveman tv.
mesmerizing.
I felt like my ape ancestors as I picked the dried flecks of meconium and blood out of her hair while she nursed (no hospital baths, please!). i ran my fingers across her warm, peach-fuzzed skin, and i held her close like the treasure and hard-won victory that she was. her latch was good, and she snacked frequently on colostrum, the golden-colored first food that a parent’s body makes while waiting on milk to come in.
bliss.
***
In my stay in the mother/baby unit, there were multiple trips to the bathroom, which for me involved the dance of hoping i’d make it and not wet myself while yanking the giant postpartum underwear/pad/coldpack combo down as fast as i could. i couldn’t feel anything at first—couldn’t feel when my bladder was full, couldn’t feel an urge to pee, could barely control peeing when i did go. try pairing that with also attempting to wait for water to get warm so you can fill a peri-bottle (which looks like something you’d bring ketchup to a picnic in) and spritz your bits while you go so it stings less, and you have physical comedy at its best. isn’t funny at the time though.
that was our first night. trying to rest, trying to pee, succeeding at nursing, succeeding at being smitten.
may 2nd, a tuesday
i wouldn’t say that we “woke up” tuesday morning so much as tuesday just kind of happened in the rhythm of nursing (me) and diaper changes (stephen) every 3 hours, vitals every 4, and clumsy and painful bathroom trips ad nauseum. feeling had come back in my perineum and everything was tender and swollen. i felt like i had massive bruising on the inside of my sacrum, and there was incredible pain and pressure behind my stitches. at some point mid-morning, while stephen was out to find breakfast, i had a nurse practitioner check everything out—she said it was a “beautiful repair”, but i felt like i’d sat on a landmine and that something was definitely *the matter*.
after the check, i ordered my own breakfast to the room and remembered thinking that a first morning postpartum deserved better than a dry sausage patty on an English muffin, a yogurt cup, a fruit cup, and bad coffee with shelf-stable creamer. (what do you want for $2500 a night, though?)
i had labs rerun to assess the extent damage caused by my hemorrhage. the biggest marker anyone is interested in is hemoglobin (the thing that’s low when you’re anemic), since it’s the molecule on red blood cells that carries oxygen. hemoglobin = body’s ability to oxygenate itself and therefore thrive, repair, and in my case, make the milk that I expected to come in in 2-3 more days. normal for women is 12-14, and i’d come into the hospital with a stellar 13.5. the loss, after one transfusion, had knocked me all the way down to an 8, just one point above needing another blood transfusion. i felt every missing point in my bones and would need a series of iv iron infusions in the coming weeks to approach normal once more.
***
after breakfast and more postpartum busyness (birth certificates, paperwork, lactation rounds, oh my!), i experienced the most transformative kindness of my whole visit. a nurse midwife who had read my chart stopped by to check in on me in case i needed someone to hold space for me to start to process what had happened. she listened. she asked honest, open-ended questions and responded with true and tender empathy. she sat masked at the foot of my bed, unhurried. she was my chaplain (also, where the fuck was the chaplain after a traumatic birth?) (also also, microsoft word has flagged “where the fuck” as “language that may be offensive to my reader”. tender reader, deal with it.)
of all the faces i saw there, hers i will remember despite only seeing half of it. she’s the only provider whose name i remember. she made herself a human to me, and she made me a human again after a traumatic experience. thank you, thank you, kate emerdello for humaning with me and with stephen when we needed it so much and for *not* treating my extraordinary experience as an ordinary work tuesday.
***
later in the morning, stephen accompanied ruby to the nursery for her newborn metabolic screen (heel poke), critical congenital heart defect (cchd) screening, and newborn hearing screen. cchd and right ear were perfect; ruby’s left ear flagged a referral and they made an appointment for us to come back later to determine whether her ear was just plugged with gunk or there was an actual hearing issue.
at 12:50 that afternoon, we dressed our daughter for the very first time (a cute blue and white floral jumper, a delightfully too-big pastel rainbow knit hat, and a pilfered hospital blanket) moved her from her hospital bassinette-on-wheels to the car seat (harrowing the first time!), and then we left for home. i must have looked an absolute fright being wheeled down the hospital corridors in my chair, hips cocked to one side to avoid putting pressure on the massive pad and cold pack over my stitches, un-showered because I preferred to bathe in my own space, crazy hair in a dirty rehabbed bun, skin an odd sort of gray-green from the massive blood loss.
crazy-pants.
surely passersby would cut me some slack since stephen (also unwashed) followed behind toting a brandinew babe and our bags. at least no one knew one bag had an on-ice human placenta in it. HA!
i was so wiped at that point that i don’t remember much about the ride home besides sitting in the back with ruby, watching her sleep, enrapt. she only woke once to express her displeasure at our decision to stop for coffee. (to this day, just about the only time she cries in a car is in a dunkin drive thru.) when we got home, i was so overtired that i was seeing things moving in my peripheral vision. i was a human battleground for sequential ocular migraines (a painless but annoying visual experience) and waking hypnic jerks. a hot mess.
i crashed into my very own bed, still double-sheeted from the anticipated home birth, knowing that i’d have to wake up in two to three hours (and in two to three hours after that, and in two to three hours after that…). the coming weeks would bring slow, agonizing healing, milk that didn’t come in due to the blood loss, a fear- and gratitude-filled dance finding milk donors, and subsequent (temporary) worries about bean’s weight… but my first-night-home sleeping self thankfully didn’t know it.
all i knew was that stephen and i had wandered into the desert and back out again over the previous year in an effort to complete our family; that the bean who we found was absolutely, positively perfect; that a good solid team of people can get you through most anything; that birth (as is always the case) hadn’t gone at all as i had imagined; and that i had absolutely, positively rocked the living shit out of it anyway. achievement unlocked.
end of chapter one.
tl/dr: planned home birth became a hospital birth when we found meconium at 4 centimeters. excruciating back labor necessitated an epidural, but it went well and ended in a lovely vaginal birth. massive 2600cc postpartum hemorrhage wrecked my train, and beanie-weenie’s noggin wrecked my bits. in the end, all were well, and my heart grew three sizes that day.