when i was 25, i had pertussis, aka whooping cough. i’d been vaccinated against it as a kid, but like most young adults, i’m positive i was AGES behind on boosters. couldn’t tell ya (before then) when the last time i’d had a t-dap was. high school? middle school? anyway, i’d caught it in the petri dish that was the university of alabama, and it was miiiiiiiserable. i didn’t have health insurance at the time (and for a long time i didn’t know how serious my “cough” actually was), so i didn’t go to the doctor. i was in grad school at the time, and i unproductively and uncontrollably coughed my way through research and bibliography, pedagogy, and spenser (sorry, ua english). could. not. stop. choking, tears rolling down my face. low-key always there. i coughed all night every night. sometimes until i dry heaved. i was worried i might break a rib. neither stephen nor i slept well for 5 weeks.
so eventually this situation became so untenable that i made an appointment at the student health center on campus. the discount doc. the place you never want to go. although no longer housed in russell hall, it was still lovingly known by ua long-timers as “russell student death center”. after waiting the requisite 2 hours (coughing the whole time), i was called back and saw the doogie howser on duty that day. he listened to my symptoms, interacting intensely with his charting, and he looked up long enough to ask, “…have you thought about losing some weight?”
he swabbed me (covid-style brain swab) and sent me home with an antibiotic (that eventually helped) and a giant bottle of codeine cough syrup mixed with lidocaine (that wound up going the the trash). no recommendation to quarantine, no instructions to stay away from others… just a crucial reminder that i was basically a walking time bomb of fat. (and had i noticed?)
i start with this story because it’s one with which i and many people are so. very. incredibly. familiar. regardless of consent to conversation, regardless of relevance to the current complaint, fat people (my preferred nomenclature, with deepest respect to the preferences of others) are aaaaaaalways proselytized to by the vague and moralizing cult of “the healthy”.
sidenote props: before i talk any more about life as a fat person, i want to acknowledge that my family absolutely never body shamed, which is apparently quite precious and unusual based on my conversations with other humans. weight was never, ever a marker of worth or something that needed to be changed in my home, for which i am thankful and owe the shred of physical self esteem that i escaped my first two decades clutching (and which subsequently grew into something fine and thriving when adult me dgaf-ed hard at that mess from the rest of the world). i was never weight shamed by my pediatrician, dr. snyder, and my first endocrinologist as a teen, dr. ovale, told me that big thighs and a big rear weren’t poor metabolic health markers. my current np is a dream, as are the folks in my obgyn and fertility practices, but the 20 years of healthcare that i received between those bookends has been a big fat (haha) train wreck.
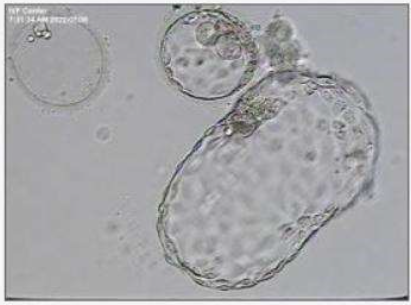
so, fast-forward to 2021. when we started thinking about ivf treatment, and entertaining the possibility that we could raise enough money to do it (average cost to a live birth in the usa is $34,400.00), i did what any reasonable human would do–i reached out to the local fertility practice here in maine with some questions. i’d learned the power of stating needs, boundaries, and goals for care ahead of time from previous interactions with my obgyn team at coastal women’s health, who without fail remember each time that i decline to be weighed (win!!), so i was proactive with my questions to the local practice.
*i only want to be weighed when it directly and provably impacts medication dosage.
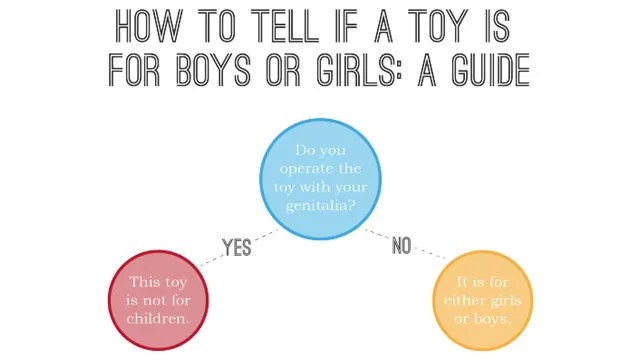
*i decline discussion about bmi, a racist tool developed by mathematicians, not doctors, for the purpose of studying populations, not people.
*i regularly hike 4000 foot mountains and run train for half marathons–i decline “exercise counseling”.
*i have an 80/20 whole foods diet and a deep understanding of nutritional principles (and of the inherent problems of “nutritionism” in western culture)–i decline “nutritional counseling”.
*will this practice accommodate my goals in a shared decision-making model?
their answer: we actually have a bmi “cut-off” over which you will be required to have regular nutritional counseling at additional expense, and your insurance is unlikely to cover you for fertility treatment anyway over that limit (completely untrue, and a scare tactic). there’s also a total bmi cutoff over which you aren’t a candidate for fertility care at all here because it “isn’t safe” (meaning they aren’t trained to manage it). we will weigh you at each visit because we “want you to be healthy and have a healthy pregnancy” (please note, this person does not have my BP, cholesterol, blood glucose, or metabolic panel levels–they’re simply referring to assumed body shape).
this call sent me first into a red rage and second to the next closest clinic in new hampshire for a second opinion. same thing, with a slightly higher bmi cut-off.
fun side note: fertility clinics will often “require” people to lose weight, even going so far as to recommend risky and drastic gastric bypass surgeries that remove whole sections of someone’s digestive system, leading to nutritional deficiencies and relying on starvation and massively disordered eating to achieve what are usually temporary results with lifelong side-effects. even people whose “biological clocks are ticking” have docs suggest wasting 2-3 years of time for surgery, loss, and restabilization before they can be eligible for (read: deserve) fertility care. unacceptable.
the real drives here? moralizing about weight (because we’re really good at that), and keeping clinic success rates high for marketing purposes.
so, you might ask, if fat people have less success with ivf, is the concern legit?
surprise, surprise. it’s complicated.
there are certain metabolic conditions like pcos that both make ivf (and conception in general) more difficult aaaaaaand cause someone to gain weight. “being fat” doesn’t give someone pcos–the syndrome that results in long anovulatory cycles and testosterone dominance also includes differences in insulin sensitivity that cause weight gain, especially in the midsection.
i don’t have pcos. (AND people who do deserve good fertility care)
then there’s hypertension, which can complicate both fertility treatment and pregnancy. fat people are more likely to have hypertension than the general population, but there are medications and lifestyles changes that can address many types of hypertension without the focus being on “weight loss”.
i don’t have hypertension. (AND people who do deserve good fertility care)
then there’s type 2 diabetes, which through a number of factors affects fertility rates and pregnancy health. around 85% of people with type 2 diabetes have what the us medical system considers a problematic/unhealthy weight.
i don’t have type 2 diabetes. (AND people who do deserve good fertility care)
so where does that leave us “fatties without comorbidities”–the people who inhabit societally unacceptably large bodies but who don’t have other markers associated with “lack of health”? and how can we continue conversations that unquestionably include and center the experiences and needs of people who do have other comorbidities. i don’t get a prize for being a “healthy fatty”–i’m a human deserving of healthcare like every. other. human. here.
but for the sake of thorough exploration, what, if not blood pressure, glucose, and metabolic disorder would give large-bodied folks poorer fertility outcomes? let’s consider…
*fat people are less likely to seek preventative care like regular check ups and cancer screenings
*fat people are more likely to have poor/distrusting relationships with medical providers because of both overt and subtle expression of provider bias (or even disgust) over a lifetime
*fat people are less likely to be believed when they report food intake, body movement, and lifestyle factors
*fat people are often 5-10 years behind their thin counterparts in disease diagnosis because all symptoms are so often attributed to/blamed on their weight
*fat people don’t have access to the critical care they need without jumping through moralized hoops around “needing to lose weight” before having access to care
*fat people encounter a lack of appropriate medical equipment when needed (bp cuffs that are too small will read abnormally high, needles that are too short might not get medicines into muscle tissue, etc.)
*fat people have increased rates of anxiety and depression related to the consumption of medical care because episodes of care so often contain shaming, even when weight is not the focus of a visit
*provision of care is often preceded, out of provider-espoused necessity, by massively disordered eating in an attempt to lose weight (which both causes an inflammatory state in the body and fails to result in lasting change over 95% of the time)
i could go on and on and on.
just “being fat” is not a risk factor. being “treated like a fat person” though absolutely is.
side note: it’s not at all the same thing, but on a related note, i always tried to train my students to replace “the lifelong experience of systemic racism” when they read “african american” or “black” as a risk factor. 99 times out of 100, that’s really what the data reflects. similar situation here. occasionally, being fat causes problems. often, problems cause being fat. always, reception as a fat person explodes the whole situation.
***************
i feel like this has been a really winding but important deep-dive rationale for why, in addition to cost, we ultimately chose cny for our fertility care. i knew after my first couple of local phone conversations that care with either of these two local places was going to feel bad. what i was looking for was scientific assistance with fertility, and what they were going to provide was morality based, evidence-scarce pressure to change myself. instead of relaxing and focusing on ivf, i’d be stressing and straining to lose weight and needing to “prove it” at weigh-ins. fuuuuuuuuck that.
and you know? i’ve done that. i weighed 260 when stephen and i were first together. didn’t get pregnant. i lost 80 pounds before our wedding. didn’t get pregnant. i crept back up to 275 in the seven years following. GOT PREGNANT. i lost 75 pounds. GOT PREGNANT. i lost 45 more pounds. didn’t get pregnant. my weight, she ain’t the problem.
in my first phone call with cny, which was with the nurse practitioner overseeing my care plan ahead of egg retrieval, she actually didn’t mention my weight at all. given my history with healthcare providers, this was so uneasy to me that i actually brought it up.
me: “do you think my weight will affect my chances and my care?”
her: *looks at chart* “oh gosh no, i don’t think so. not at all”
me: “do you require nutritional counseling?”
her: “does that feel important to you or like it would be helpful?”
me: “no, i’m a midwife and a health-minded person with decent access to resources, so i’m good”
her: “then absolutely no, not unless that’s a goal for you”
(ensuing conversation about the toxic nature of medical fatphobia)
in the entirety of my care at cny, i self-reported weight once on an intake form, and last week the nurse asked me to “just grab a quick weight before surgery so the anesthesiologist would know how much propofol to give me”. that’s it. no moralizing. no gatekeeping. no patronizing. no shaming. data gathering when data was needed. and there’s plenty of information available through the practice about eating for health and fertility, but it’s all simply available on offer, not a required regimen or forced discussion.
game changer.
and cny does this at professional cost, though it doesn’t seem to be hurting them. they take people regardless of age and regardless of weight (both of which are definitely not the norm) with the full understanding that this will make “their numbers” not their selling point. their philosophy is affordable, personalized, informed care for all, and i am delighted to report that it’s been a life-changing experience for me.
it’s a tender and vulnerable thing, but i invite you to share your stories, in the comments below, of times you received very poor or very exceptional care in a body that deviates from our narrow views of healthy. what was the experience like? how did it affect you? has it changed the way you advocate for yourself?
thank you in advance for your your candor and vulnerability in sharing experiences.
yours truly,
a hopeful (fat, and healthy) mama